Chronic Pancreatitis
Chronic Pancreatitis
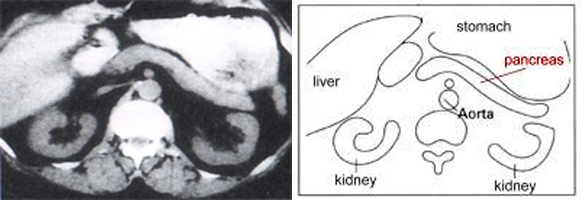
Normal pancreas: at left: picture of a computerised tomography (CAT Scan) with normal healthy organs; at right: diagrammic presentation
What is chronic pancreatitis?
Chronic pancreatitis is the chronic (long-term) inflammation of the pancreas. Repetitive and long-lasting relapses of inflammation gice rise to a progressive destruction of healthy cells. These are replaced by scar tissue and, as a result, the pancreas can no longer perform its functions fully.
1. The production of digestive enzymes, which are essential for breaking down food for absorption into the body ceases. This leads to diarrhoea (often foul-smelling) weight loss and vitamin deficiency.
2. Also, as the pancreas' islet cells are destroyed, less or no insulin is manufactured, the metabolising of glucose is disrupted and diabetes mellitus develops.
The main symptom of chronic pancreatitis are severe pains in the upper abdomen. These pains often radiate around to the patient's back and are probably caused by changes in the pancreatic nerve tissue, and/or by blocked fluids in the pancreatic ducts. This will bring about an ever-increasing pressure in the pancreas. Pains can also be caused by the obstruction of processed foods in stomach and intestines or massive bloating. Even strong medication can not always eliminate the effects of these severe pains.
Main duct of the pancreas. ERCP-pictures that show different stages of a chronic pancreatitis, increasing from top to bottom.
What are the causes of chronic pancreatitis?
In the west, excessive alcohol consumption is the common cause (80%) of chronic pancreatitis. However, not all cases are due to chronic over-consumption. Patients have varying degrees of alcohol tolerance, and in some cases the disease is triggered when consuming relatively small amounts.
Besides alcohol, there are other important causes for the disease. These include a tendency to chronic gallstones, genetic defects, certain conditions in the pancreatic ducts (pancreas divisum), medication and disorders of the metabolism. Sometimes, no particular cause can be found.
What are the most frequently encountered symptoms of chronic pancreatitis?
- Pains
- Bloating
- Diarrhea
- Weight loss
- Diabetes mellitus
Pictures of a Chronic Pancreatitis
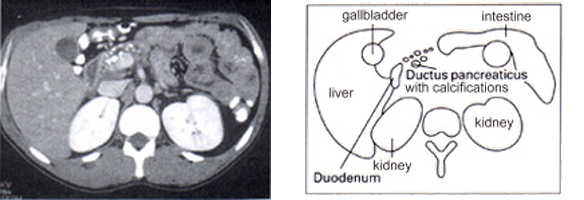
Picture of a computerised tomography (CAT Scan) or a sketch show a enlarged pancreatic duct in the body of the pancreas, with calcination.
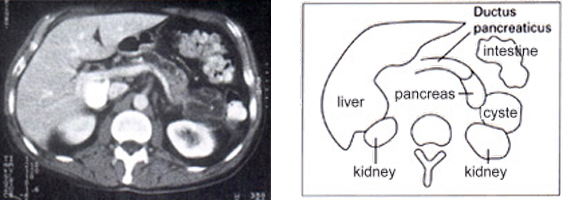
This picture of a computerised tomography (CAT Scan) or the sketch show a cyste at the tail of the pancreas.
The Treatment of Chronic Pancreatitis
Treatment is determined by the patient's symptoms. Often, patients suffer from almost unbearable pains in the upper abdomen. Alcohol consumption must be discontinued as a first measure. Pancreatic enzyme supplements can then be taken, alleviating the condition by suppressing pancreatic secretions (thus relieving the pressure on the pancreas) and restoring the digestive process. If this does not alleviate pains, medication should be the next option. Failing this, surgery must be considered.
Fatty deposits in the stool and/or diarrhoea are proof that the pancreas is not producing sufficient digestive enzymes. These must be substituted with a regular intake of an appropriate medication. The presence of the condition may also be verified by a pancreatic enzyme (elastase) found in the patient's stool.
Fat content of the meal will determine how many capsules containing enzymes need to be taken. To ensure that these have the desired effect it is often necessary to stem the stomach's natural acid production with acid-blocking medication. It is also vital to ensure the patient takes a sufficient amount of fat-soluble vitamins (A, D, E, K). In some severe cases, these may have to be injected. A blood test will show whether this is necessary.
A rising blood sugar level is proof that not enough insulin is produced in the pancreas. Dietary measures alleviate this condition in a few cases only. Patients routinely need to take additonal doses of insulin to regulate blood sugar levels.
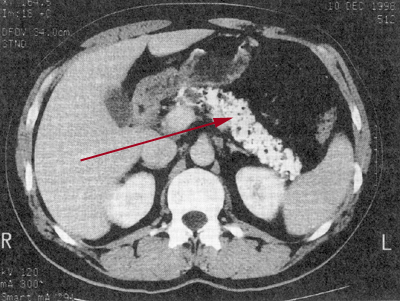
Calcification (arrow) with a chronic pancreatitis.
When is an operation required?
50% of patients with chronic pancreatitis will require surgery at some point. As the procedures are very complicated, pancreatic surgery will usually be performed in specialised clinics. Several reasons demonstrate why surgery is necessary:
1. Pain management is unsuccessful, even when using the most potent
medication.
2. A chronically inflamed pancreas affects surrounding organs such as the duodenum (constraint or blockage), the bile duct, the main pancreatic duct and blood vessels behind the pancreas.
3. Suspicion that the condition masks pancreatic cancer.
Pseudo-cysts (cavities filled with fluids, caused by inflammation) are sometimes found. Filled with pancreatic fuids, they are located next to or in the pancreas and will often vanish without medical intervention. However, they can become enlarged and will cause problems locally. They must be surgically removed or drained. When best to have the operation has to be discussed with An experienced pancreatic surgeon will determine the proper timing for surgery. A timely removal will restore the functions of the pancreas (digestion, blood sugar control).
What happens during surgery?
Surgical procedures can be used in two different ways: removal or draining. The nature of alterations in the pancreas will determine which is the preferred route. When using surgical draining the physician opens the main pancreatic duct fully and connects the pancreas to the small intestine. This enables pancreatic juices to flow directly into the intestines. If a cyst is found, it is opened and connceted to the small intestine and blocked fluids are released.
Often, recurring inflammations will have reduced organ function to such an extent that this procedure will not permanently improve the condition. If pains persist, damaged sections of the organ will be removed permanently.
The head (usually most severely affected) will be removed first. Surgeons will proceed with utmost caution, removing only badly damaged tissue. Neighbouring organs such as duodenum, gall ducts and stomach are not affected during the operation.
In special circumstances removal of these organs may be necessary as well. The tail piece of the pancreas may be removed if inflamed. This is done without affecting the spleen if possible. After removing damaged pancreatic tissue, a section of small intestine will be sewn on to the remaining part of the pancreas, so digestive fluids can be released.
Pancreatic surgery is extremely demanding and technically difficult. It should therefore only be performed by qualified surgeons in larger and specialised clinics.
Part of my pancreas has been removed - what next?
Patients who have had part or the all of their pancreas removed will experience a reduction of the pancreas function, depending on how much of the organ had to be removed. This will cause the following deficiencies:
- Not enough pancreatic enzymes (digestive disorders)
- Insuffiecent insulin production (high blood-sugar levels)
These deficiencies can be addressed by taking appropriate medication.
Pancreatic Enzyme Substitution
At present, drugs which substitiute pancreatic enzymes are available. They must be taken with all meals and snacks. Correct doses vary from patient to patient and are determined by nature of food taken and by symptoms present in the patient. Bloated feelings and diarrhoea with excess fatty substances can be addressed and handled with these drugs. More capsules need to be taken with main meals than with snacks. Enzymes must be in direct contact with food in order to be effective and 6-12 capsules per day are needed. The doses may vary significantly and are governed by the nature of the drug (amount of enzymes contained in one capsule) and the remaining function of the pancreas.
Substitiute enzymes are readily asborbed into the body and patients do not suffer any side-effects. In very rare cases, the drug can cause an allergic reaction.
Insulin Substitution
If a pancreatic disorder or surgery has caused high blood sugar levels, patients will require some form of blood sugar level correction. Initially, and if levels are not severely elevated, this can be achieved by nutritional means and with medication capable of influencing blood glucose levels. However, insulin treatment may be necessary if the amount on insulin producing cells in the pancres has been reduced significantly. Treatment can be tailor-made to the requirements of the individual patient, as a variety of insulin types are now available. Thus, the patient's nutritional preferences can be respected. The goal of any such treatment is the well-being of the patient and efficient managing of blood sugar levels. Thus, doctors can avoid severe damage over the short and longer term. Close supervision by a GP or specialist is required in the initial phase of the treatment.
My spleen has been removed - what next?
Sometimes the spleen is removed during pancreatic sugery.
The spleen supports the immune system. If removed, a person is more susceptible to bacterial infections, some of which can cause life-threatening diseases. To protect patients against this threat, inoculations must be administered. Pneumococcal infections and vaccinations against this particular disease must be mentioned here. According to current research, patients need to receive these inoculations again after about 3 to 5 years. Patients need to visit their doctor when suffering from infections and fever, and inform medical staff that they do not have a spleen. The physician will decide whether a treatment with antibiotics is warranted.
Removal of the spleen can lead to a build-up of blood platelets (thrombocytes). It is important to keep an eye on this. Blood thickening and possibly thrombosis can result if the number of platelets is elevated to risk-level. Should this occur, your doctor will prescribe medication to reduce the risk of thrombosis.
to top
