Pancreas
Pancreas
What is the Pancreas?
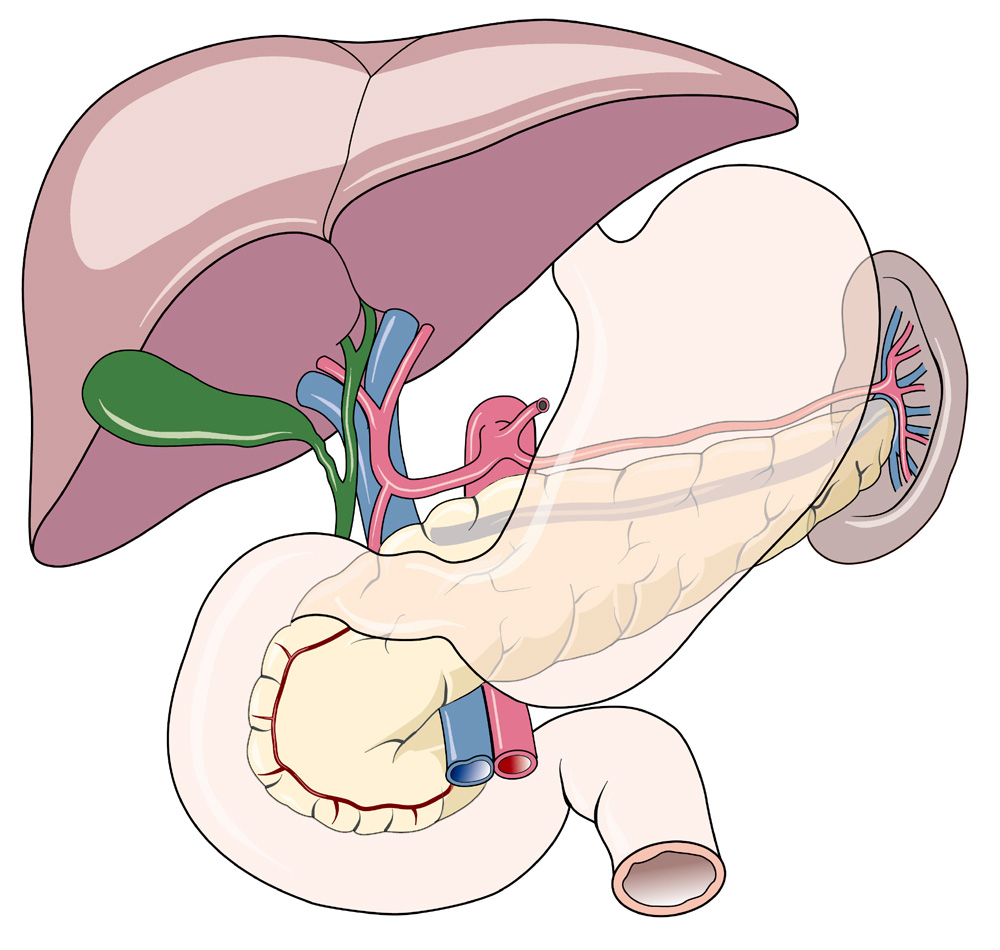
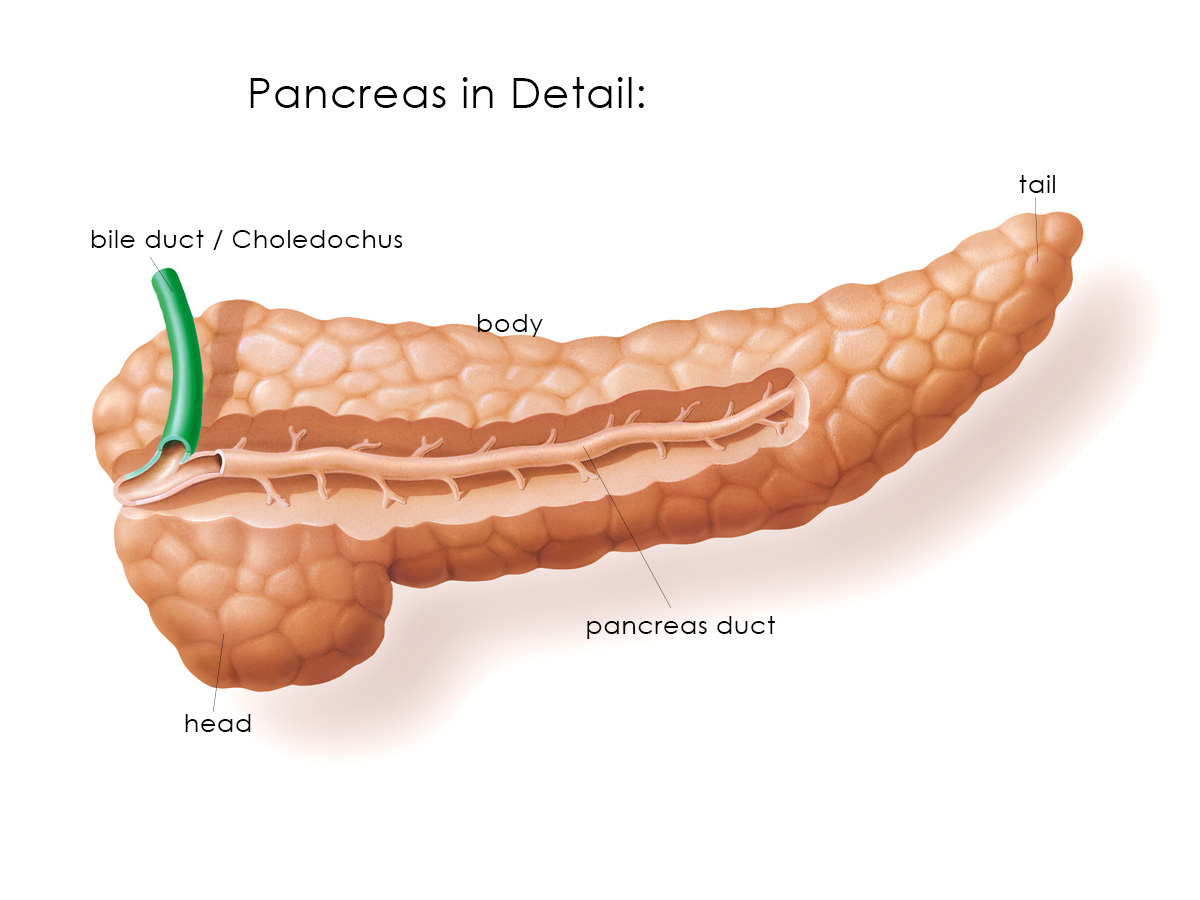
The pancreas is an yellowish gland, ca. 15 cm long, 5 cm wide and 2-3 cm in diameter. It can be roughly divided into three parts: the head, the body and the tail (Fig. 2). The pancreas head is closely connected to the first part of the small intestine, known as the duodenum . The pancreas tail extends to the left part of the spleen . The body of the pancreas is located before a junction of a number of important blood vessels leaving the aorta . They supply blood to the liver, the stomach, the upper part of the intestine and the pancreas itself.
The location of the pancreas
What does the Pancreas do?
The pancreas has two functions:
1. It is crucial to the function of the digestive system (exocrine function).
2. It controls blood sugar levels.
The Pancreas and Digestion
The pancreas manufactures important enzymes . 1.5 - 3 litres of a secretion saturated with enzymes are produced on a daily basis. 60 g of protein are metabolised in the process, which amounts to an enormous output. Specialised cells located throughout the entire gland produce the secretion. At first, a preliminary version is produced and pumped into a vast system of ducts from where it is released into the main duct (known as ductus pancreaticus). Bile secretion (produced in the liver) merges with the pancreatic secretion shortly before the mixture flows into the duodenum, at a point, which is known as Papilla Vateri. Pancreatic enzymes are activated at this point and receive their full digestive functionality. Food passed by the stomach can now be digested.
The pancreas produces more than 20 different digestive enzymes. They break down food into small elements. Although the enzymes are produced in the pancreas, they only become functional in the duodenum. Therefore they will not digest the pancreas itself.
The three most important enzymes produced in the pancreas are:
- Amylase: digests carbohydrates
- Trypsin: digests proteins
- Lipase: digests fats
Breaking down food into components is necessary so the body can absorb these through the intestines. In the absence of the pancreatic enzymes sugars, proteins and fats will not be broken down properly and the intestines will not be able to absorb nutrients into the bloodstream, causing diarrhoea, bloating and abdominal cramps. Persistent weight loss, vitamin deficiencies and malfunctioning of other organs will also occur, as nutrients cannot be absorbed and the body therefore lacks the required energy.
The Pancreas and the Regulation of Blood Sugar
Aside from digestive enzymes, the pancreas also produces an important hormone , known as insulin . Insulin is manufactured in special groups of cells, known as the Islets of Langerhans, found throughout the pancreas. They account for only 2.5 g of the total weight of the pancreas (80 - 100 g). There are about 1.5 million of these cells. The insulin is secreted from these cells in the pancreas directly into the bloodstream. It is crucial in the control of blood sugar levels. Glucose is the most important of all sugar molecules. All cells depend on glucose to retain their functionality. After reaching the bloodstream through the intestines, blood sugar enters the individual cells with the help of insulin.
Blood sugar cannot enter the cells if there is not enough insulin (or none at all) in the bloodstream. If this condition is present, blood sugar levels rise constantly, leading to unpleasant or even life-threatening consequences. Diabetics suffer from varying degrees of insulin deficiency.
Another important hormone produced by the pancreas is known as glucagon. This hormone is also manufactured in the insulin cells. Glucagon counteracts insulin in the body. When cell life is threatened by a lack of blood sugar, glucagon releases residual blood sugar from elsewhere in the body, particularly the liver. In the absence of the pancreas (i.e. after surgery), the glucagon hormone can no longer be produced. This factor must be considered when caring for pancreas patients.
The production of pancreatic enzymes and insulin are by and large separate processes. If damage is done to the pancreas, both functions may be disrupted independently.
Pancreatic malformations
During embryonic development, the pancreas arises from two separate parts, which move together as the embryo is growing.
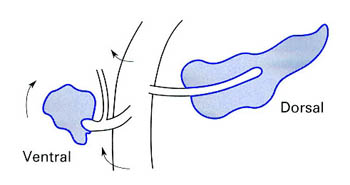
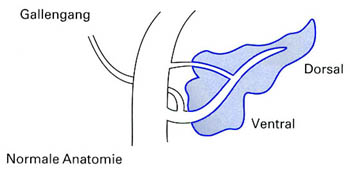
During this process, both parts of the gland including the separate ducts fuse to a form single organ. The originally more ventrally located part of the pancreas moves to the back.
 <
<
Disturbances during the embryonic development of the pancreas can lead to two clinically important malformations i.e. annular pancreas and pancreas divisum.
1. Annular pancreas
During normal development, the two separate ductal systems of the pancreas fuse to form a common duct. In case of pancreas divisum, these two duct systems do not fuse in spite of the development of a single organ. As a result, there are two separate pancreatic ducts that drain into the duodenum.
Subsequently, the pancreatic duct from the dorsal larger part of the pancreas drains through the so called Ductus Santorini via a small opening called the small (minor) Papilla. The ventral pancreatic duct drains the pancreatic juice via the so called Ductus Wirsungianus through the major opening called Papilla major. In this area, there is also the opening of the bileduct (Ductus choledochus).
2. Pancreas divisum
During normal development, the two separate ductal systems of the pancreas fuse to form a common duct. In case of pancreas divisum, these two duct systems do not fuse in spite of the development of a single organ. As a result, there are two separate pancreatic ducts that drain into the duodenum.
Subsequently, the pancreatic duct from the dorsal larger part of the pancreas drains through the so called Ductus Santorini via a small opening called the small (minor) Papilla. The ventral pancreatic duct drains the pancreatic juice via the so called Ductus Wirsungianus through the major opening called Papilla major. In this area, there is also the opening of the bileduct (Ductus choledochus)
.
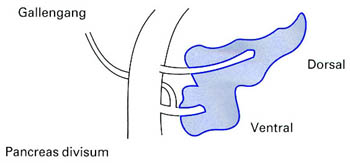
This anatomical variation occurs in between 3 - 10% of the general population. In most cases this variation does not cause any symptoms. However, if the minor Papilla is too narrow, there is inadequate drainage of the pancreatic juice into the duodenum leading to acute or chronic inflammation of the pancreas.
The first line of treatment in this condition is to widen the opening of this pancreatic duct. It can be achieved endoscopically by making a small cut into the minor Papilla, sometimes together with the introduction of a small tube. While some patients benefit from this treatment, symptoms relapse in most patients.
Nowadays, the treatment of choice is an operation where parts of the openings are excised surgically without removing any part of the pancreas. Most patients undergoing this operation experience long term symptom relief.
to top
