Acute Pancreatitis
Acute Pancreatitis
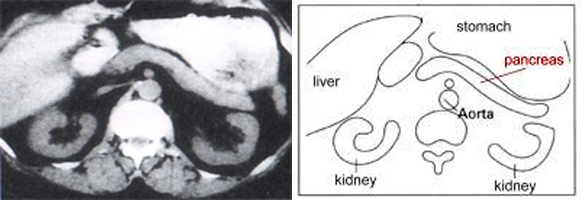
Normal pancreas: at left: picture of a computerised tomography (CAT Scan) with normal healthy organs; at right: diagrammic presentation
What is acute pancreatitis?
Acute pancreatitis is an acute, i.e. suddenly occurring, inflammation of the pancreas. It results in damage to the cells of the pancreas, which limits its function for a temporary period. Depending on the severity of the damage, acute pancreatitis can also lead to the death of pancreatic cells, which results in various harmful substances being secreted into the body, which in turn can cause the patient to become critically ill. As the illness progresses, other organs may be attacked and their function affected. We differentiate two forms of acute pancreatitis:
1. Acute oedematous pancreatitis
2. Acute necrosing pancreatitis
At the outset of pancreatitis it is usually impossible to diagnose which of the two forms is present or developing in the patient. Thus all patients with acute pancreatitis must receive intensive care at an early stage.
1. Acute oedematous pancreatitis
This is the gentler form, and around 85% of patients with acute pancreatitis suffer from this version of the disease. It causes temporary damage to the pancreas, but does not normally affect any of the surrounding organs. In most cases, the patient recovers completely from the inflammation and there is no long-term damage to the pancreas.
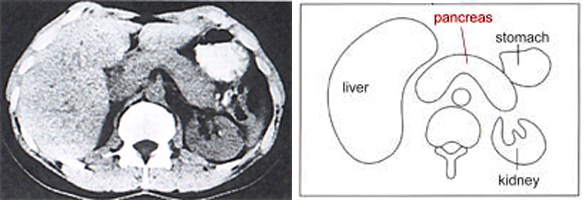
At left: picture of a computerised tomography (CAT Scan) of a distinct homogenic enlargement of the pancreas with a oedematous pancreatitiss; at right: diagrammic presentation
2. Acute necrosing pancreatitis
Around 15% of patients with acute pancreatitis suffer from this most serious inflammation of the pancreas. Sudden widespread destruction of pancreatic tissue occurs. Furthermore, failure of other organs such as lungs and liver can often seriously endanger the patient's life. As a consequence of the disease, the function of the pancreas is in most cases permanently reduced, leading to digestion disorders and/or diabetes. Loss of function is proportionate to the amount of destruction of pancreatic tissue. Defunct tissue can also lead to problems in the abdomen, such as pseudo-cysts, abscesses and obstruction of fluids in the ducts of the gall, as well as in the stomach or intestines. These complications have to be individually assessed and treated according to their severity, they often necessitate surgery.
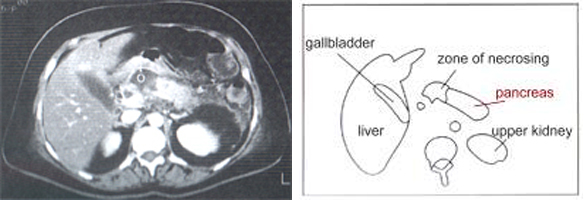
At left: picture of a computerised tomography (CAT Scan) of a necrosing zone; at right: diagrammic presentation
What are the causes of acute pancreatitis?
There is a long list of possible causes of acute pancreatitis. However, in Central and Western Europe, gallstones and excessive alcohol consumption are responsible for 90% of cases. Metabolised alcoholic substances can damage pancreatic tissue directly. If a gallstone passes from the gall bladder to the common bile duct, it can block the pancreatic duct (which joins the common bile duct shortly before the duodenum), and this can lead to acute pancreatitis. In addition to these common causes, there is a whole host of much rarer causes, such as infections, various forms of medication, and congenital defects in the pancreatic ducts. Finally, there is also a small number of cases, where to date no cause for pancreatitis has been found.
What are the symptoms of acute pancreatitis?
- Sudden onset
- Severe, dull pain in the upper abdomen (often radiating around to the patient´s back, like a belt)
- Nausea, vomiting, bloated feeling
- High temperature
Treatment of acute pancreatitis
Treatment of acute pancreatitis is largely determined by the patient's symptoms and varies according to the form of the disease (mild or severe). In general, patients with acute pancreatitis need to be monitored and treated in hospital. The patient will be prevented from eating or taking fluids for a number of days to allow the pancreas to recuperate. Pain relief and fluids via intravenous drip will be administered. The circulatory system, lungs and kidneys will be monitored carefully. Nutrition can be phased in if treatment is successful. Intensive care must be administered if the severe form of acute pancreatitis is found. Restoring and monitoring organ function is imperative.
What cases require surgery?
One out of three patients with acute pancreatitis requires surgery. Surgical intervention is indicated if the patient's condition deteriorates and an infection or haemorrhage is found in defunct pancreatic tissue. The patient's abdomen in opened with a lengthwise incision, and infected and defunct parts of the pancreas are removed to prevent further infections. Finally, tubes are inserted through which the area around the pancreas is drained to prevent further infections. In severe cases of acute pancreatitis, the patient may be required to stay in hospital for several weeks.
Apart from treating the actual acute condition, physicians will also investigate the origin of the disease. Gallstones, if found to be the cause, will be removed with ERCP immediately. The flow of pancreatic enzymes and bile into the duodenum is thus restored and the immediate cause for the damage is removed. After the patient has recovered from acute pancreatitis caused by gallstones, the gall bladder will be removed. In most cases, this is done with keyhole surgery (laparoscopic cholecystectomy).
When dealing with acute pancreatitis, doctors will routinely investigate the patient's alcohol consumption. Where alcohol is the cause, excessive consumption may not always be to blame. Some people with increased sensitivity may develop acute pancreatitis after consuming moderate amounts of alcohol. Conversely, some excessive drinkers never develop acute pancreatitis. Whatever the case, it is imperative that acute pancreatitis sufferers limit their alcohol intake in the aftermath of the disease.
Long-term effects of acute pancreatitis
The following problems can arise apart from the functional damage to the pancreas (disgestive disorders due to the lack of digestive enzymes in the remaining part of the pancreas, or development of diabetes mellitus due to the lack of sufficient quantities of insulin):
1. Formation of pseudocysts
Due to tissue damage of the pancreas including the destruction of entire duct sections, a loss of continuity in the pancreatic duct system can result. Leaking pancreatic fluids or blood collect in or around the pancreas. This collection of pancreatic fluids, blood, and dead tissue, which is found in or on the pancreas, is called a pseudocyst. They often disappear without any therapy; however, there are pseudocysts which get bigger and bigger resulting in complaints such as nausea, vomiting, pain, and weight loss. It can also happen that the passage of food in the stomach or intestines is hindered or the flow of bile is obstructed. Finally, there is the danger of them rupturing and emptying into the abdominal cavity. Pseudocysts causing symptoms, generally require surgery in which a section of the small intestine is opened and stitched onto such a pseudocyst, enabling the cyst contents to drain directly into the intestine. Often, an endoscopic drainage can be performed as well.
2. Pancreatic Abscesses
Sometimes, in the aftermath of an acute inflammation, an accumulation of pus can occur in the pancreas area, causing instances of recurring high temperature. Normally, the physician can puncture the abscess under a local anaesthetic (closely monitored by ultrasound or CAT). Pus can then be removed via catheter. If this is impossible, surgery will be required. The patient will also need antibiotic treatment.
Part of my pancreas has been removed - what next?
Patients who have had part or the all of their pancreas removed will experience a reduction of the pancreas function, depending on how much of the organ has been removed. This will cause the following deficiencies:
- Not enough pancreatic enzymes (digestive disorders)
- Insufficent insulin production (high blood-sugar levels)
These deficiencies can be addressed by taking appropriate medication.
Pancreatic Enzyme Substitution
At present, drugs which substitiute pancreatic enzymes are available. They must be taken with all meals and snacks. Correct doses vary from patient to patient and are determined by nature of food taken and by symptoms present in the patient. Bloated feelings and diarrhoea with excess fatty substances can be addressed and handled with these drugs. More capsules need to be taken with main meals than with snacks. Enzymes must be in direct contact with food in order to be effective and 6-12 capsules per day are needed. The doses may vary significantly and are governed by the nature of the drug (amount of enzymes contained in one capsule) and the remaining function of the pancreas.
Substitiute enzymes are readily asborbed into the body and patients do not suffer side-effects. In very rare cases, the drug can cause an allergic reaction.
Insulin Substitution
If a pancreatic disorder or surgery has caused high blood sugar levels, patients will require some form of blood sugar level correction. Initially, and if levels are not severely elevated, this can be achieved by nutritional means and with medication capable of influencing blood glucose levels. However, insulin treatment may be necessary if the amount on insulin producing cells in the pancres has been reduced significantly. Treatment can be tailor-made to the requirements of the individual patient, as a variety of insulin types are now available. Thus, the patient's nutritional preferences can be respected. The goal of any such treatment is the well-being of the patient and efficient managing of blood sugar levels. Thus, doctors can avoid severe damage over the short and longer term. Close supervision by a GP or specialist is required in the initial phase of the treatment.
My spleen has been removed - what next?
Sometimes the spleen is removed during pancreatic sugery.
Life is possible without spleen. The spleen supports the immune system. If removed, a person is more susceptible to bacterial infections, some of which can cause life-threatening diseases. To protect patients against this threat, inoculations must be administered. Pneumococcal infections and vaccinations against this particular disease must be mentioned here. According to current research, patients need to receive these inoculations again after about 3 to 5 years.
Patients need to visit their doctor when suffering from infections and fever, and inform medical staff that they do not have a spleen. The physician will decide whether a treatment with antibiotics is warranted.
Removal of the spleen can lead to a build-up of blood platelets (thrombocytes). It is important to keep an eye on this. Blood thickening and possibly thrombosis can result if the number of platelets is elevated to risk-level. Should this occur, your doctor will prescribe medication to reduce the risk of thrombosis.
to top
